February in the US is both Black History Month and American Heart Month. In a recent post, we discussed health disparities–preventable differences in health that are experienced by socially disadvantaged populations–and the factors that cause them, or social determinants of health. Rooted in differences in quality of education to economic disadvantages, it’s well-established that Black communities in America have, overall, poorer health than their non-Black neighbors (particularly non-Hispanic white Americans). Let’s dive a little deeper and take a look at what kinds of conditions Black Americans are more likely to experience.
Table of Contents
Why Do Black Americans Experience Higher Rates of Chronic Disease?
Social Determinants of Health
Let’s Talk About Race
Genetic Basis for Disease
Cardiovascular Disease, Hypertension, and Stroke
Sickle Cell Anemia
Cancer
Obesity
Obstetric Complications
Mental Illness
Why Do Black Americans Experience Higher Rates of Chronic Disease?
Do a quick Google search for “why so many do Black Americans have kidney disease?” and you’ll probably find a few articles that cite the increased prevalence of diabetes and hypertension as the reason. But why do so many Black Americans have diabetes and hypertension? The health disparities experienced by Black communities in the US is a complex, deeply-rooted, mess of a situation that is hardly the result of one main contributing factor–although systemic racism is always a great place to start. While social determinants of health (SDOHs) are certainly responsible for higher rates of chronic disease among Black populations, there can also be genetic factors. But it’s far more complicated than “Black genes” and “white genes”–which, by the way, do not exist. Read on to learn more.
Social Determinants of Health
We covered this in more depth in a previous post, but SDOHs are worth mentioning again. Higher rates of chronic disease can be linked to socioeconomic status, education level, and access to quality healthcare. In 2022, the poverty rate for the Black population reached a record low at 17.1%--a significant improvement to historical rates like 55.1% in 1959. While this is certainly noteworthy, it’s nearly twice the rate experienced by non-Hispanic white Americans, 8.6% of whom live in poverty. Similar disparities are seen in on-time high school graduation rates. In Michigan, 61% of Black boys graduated on time in 2021, compared to 81% of white boys. High school completion rates are strongly correlated to socioeconomic status, which determines both whether a person lives in an area with quality healthcare, and if they can even afford it.
Let’s Talk About Race
Correlating race with predisposition to disease is about as complicated as everything we’ve talked about so far. When people suggest that different races experience different rates of certain diseases, it’s almost implied that this difference is because of something that is inherent to each race–something, say, genetic. Although race as we understand it today is a critical part of many people’s identity and sense of self, it’s a completely made-up concept. As the National Museum of African-American History and Culture puts it, “[r]ace is a human-invented, shorthand term used to describe and categorize people into various social groups.” In fact, when the Human Genome Project was completed in 2003, it confirmed that humans are 99.9% genetically identical. There is no genetic basis for race.
So how do we as health providers account for our Black patients’ “Blackness” in a way that acknowledges that they are nearly genetically identical to every other patient we’ve seen, while also recognizing that they are statistically more likely to experience chronic disease than other patients? You already know the answer: social determinants of health. There are valid racial considerations in medical decision-making, but these considerations are largely social and cultural. The figure below demonstrates this well. At a glance, you can easily see that Black Americans are more likely to be hypertensive than white Americans. However, for both populations, the rate of hypertension declines with greater education—something we’ve already established that white Americans are more likely to attain.
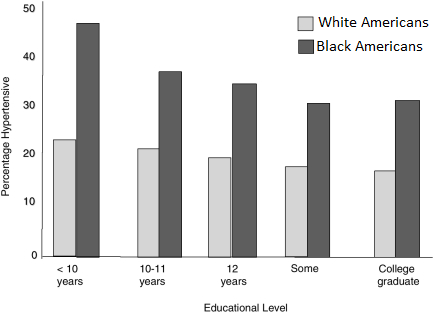
Adapted from “Critical Perspectives on Racial and Ethnic Differences in Health in Late Life.”
National Research Council Panel on Race, Ethnicity, and Health in Later Life. 2004.
Genetic Basis for Disease
First, it’s important to know that the concept of correlating genetics with disease in general is relatively new as far as the history of disease etiology and bioinformatics goes. In 2010, a study at the Vanderbilt University School of Medicine demonstrated the feasibility of linking patients’ genes to their diseases. Since then, the practice of trying to identify which genetic variations may be responsible for diseases has become more common, but it’s still not foolproof. So while genetics are known to be somewhat of a risk factor for diseases like chronic kidney disease, only a small group of people is affected by these genes, and it has little to do with their race.
Cardiovascular Disease, Hypertension, and Stroke
In the United States, 1 of every 3 deaths is related to cardiovascular disease. Although this statistic represents the rate of disease in all Americans, Black Americans are statistically more likely to experience cardiovascular disease and related conditions such as hypertension, heart attacks, and strokes. These often go hand in hand with other diseases that are more prevalent in Black communities, such as diabetes, cholesterol, and chronic stress.
Sickle Cell Anemia
Even though sickle cell anemia (SCA) is considered to be a rare disease, it affects 1 in every 365 Black newborns. For comparison, Down syndrome affects 1 of every 700 babies born in the US, and cystic fibrosis (CF) affects 1 in every 3,500 white babies. SCA is a genetic disease, and about 1 in every 13 Black babies is estimated to carry the gene.
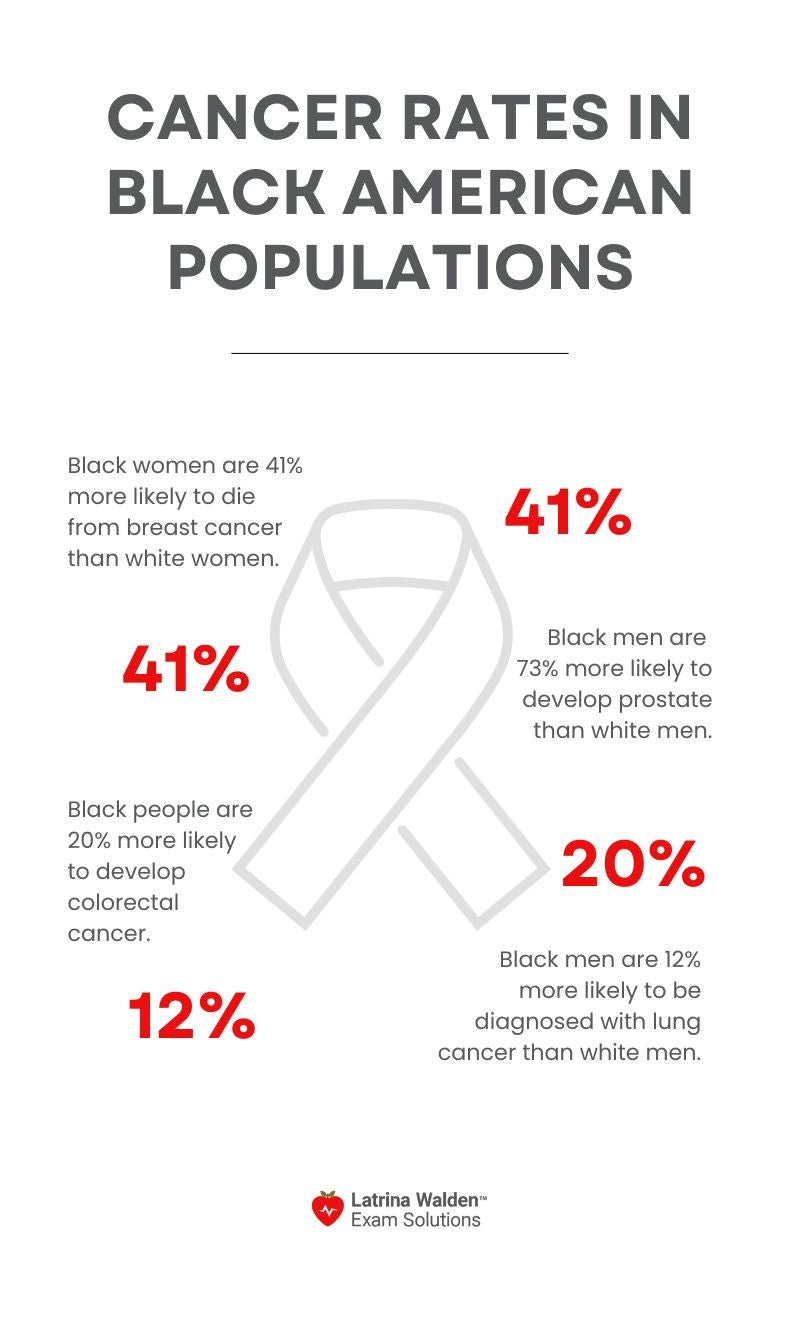
Cancer
Across nearly every cancer type, Black men and women alike are more likely to be diagnosed with cancer than white patients, and are almost always more likely to die from their cancer.
Obesity
Remember SDOHs? (How could we let you forget? 😂) This disparity is particularly linked to food insecurity. When people don’t have access to healthful, nutritious food, they are more likely to eat calorie-dense, affordable options. This results in what’s known as the “food insecurity-obesity paradox”. And as we’ve discussed, Black Americans are way more likely to experience food insecurity; relatedly, they’re 30% more likely to be obese. This can also be related to what’s known as a food desert, or a geographic area where healthful foods like fresh produce are unavailable or just too expensive for many people. In the US, 1 out of every 5 Black families lives in a food desert.
Obstetric Complications
The rate of poor (to say the least) maternal outcomes among Black women in the US is nothing short of a public health crisis, and a disgrace to a country with some of the most advanced medical technologies in the world. Black women are significantly more likely than any other racial group to have a Cesarean delivery (C-section). In 2021 it was reported that nearly 70 of every 100,000 live births to Black women resulted in maternal death–a rate that was 2.6 times higher than the rate for non-Hispanic white women.
Another complex statistic, this significant disparity be attributed to three main factors:
- Black mothers are more likely to have cardiovascular conditions that increase their risk during pregnancy.
- Black women are more likely to experience adverse pregnancy outcomes, which puts them at risk for long-term cardiovascular disease (remember when we said this was complex?).
- Racial bias of providers and distrust in the medical community in general makes Black mothers less likely to seek care during their pregnancy and after.
Mental Illness
Yet another area of health in which Black Americans suffer more than other racial groups. According to the National Alliance on Mental Illness (NAMI), Black adults in the US are more likely to experience mental illness. This is evidenced by higher rates of suicide, serious psychological distress, and reported feelings of “sadness, hopelessness, [and] worthlessness”. Despite the demonstrated need for mental health resources, only 1 in 3 Black adults with mental illness receive treatment. This is likely related to difficulty in accessing mental health resources (especially affordable ones), and increased stigma around mental health conditions.